According to new research, the brain’s map of the body remains unchanged even after a limb has been amputated, contrary to the prevailing view that it rearranges itself to compensate for the loss. The findings have implications for the treatment of phantom limb pain, but they also suggest that controlling robotic replacement limbs via neural interfaces may be more straightforward than previously thought.
Studies have previously shown that a map of the body exists within the brain’s somatosensory cortex, with different regions corresponding to different body parts and responsible for processing sensory information such as touch, temperature, and pain, as well as body position.
The commonly accepted view among neuroscientists has been that following amputation of a limb, neighboring regions rearrange and essentially take over the area previously assigned to the now missing limb. This has relied on evidence from studies carried out after amputation, without comparing activity in the brain maps beforehand, but couldn’t explain why people with amputations report phantom limb sensations and pain. Brain imaging studies where people have been asked to “move” their missing fingers have also shown brain patterns resembling those of able-bodied individuals.
To investigate this contradiction, a team led by Tamar Makin, PhD, from the University of Cambridge, and Hunter Schone, PhD, from the University of Pittsburgh, followed three individuals due to undergo amputation of one of their hands. This is the first time a study has looked at the hand and face maps of individuals before and after amputation.
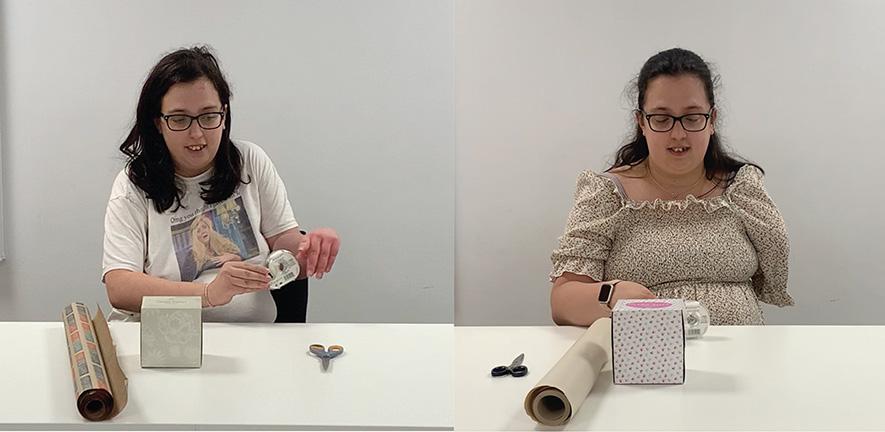
Prior to amputation, the three individuals were able to move all five digits of their hands. While lying in a functional magnetic resonance imaging scanner, the participants were asked to move their individual fingers and to purse their lips. The researchers used the brain scans to construct maps of the hand and lips for each individual; in the maps, control of the lips are near the hand.
The participants repeated the activity at three months and six months after amputation, this time asked to purse their lips and to imagine moving individual fingers. One participant was scanned again 18 months after amputation and a second participant five years after amputation.
The researchers compared the pre- and post-amputation maps and found them almost identical.
“Because of our previous work, we suspected that the brain maps would be largely unchanged, but the extent to which the map of the missing limb remained intact was jaw-dropping,” said Makin, from the Medical Research Council Cognition and Brain Science Unit at the university and the study’s senior author. “Bearing in mind that the somatosensory cortex is responsible for interpreting what’s going on within the body, it seems astonishing that it doesn’t seem to know that the hand is no longer there.”
As previous studies had suggested that the body map reorganizes, the researchers looked at the region corresponding to the lips to see if it had moved or spread. They found that it remained unchanged and had not taken over the region representing the missing hand.
To complement their findings, the researchers compared their case studies to 26 participants who had had upper limbs amputated, on average 23.5 years beforehand. These individuals showed similar brain representations of the hand and lips to those in their three case studies, suggesting long-term evidence for the stability of hand and lip representations despite amputation.
The researchers’ explanation for the previous misunderstanding about the brain map is that the boundaries within the brain maps are not clear. So while inputs from the middle finger may largely activate one region, they also show some activity in the region representing the forefinger, for example.
The new research results suggest that current approaches to treating phantom limb pain have focused on the wrong problem, which is why they have shown limited success.
“The remaining parts of the nerves—still inside the residual limb—are no longer connected to their end-targets,” said Schone. “They are dramatically cut off from the sensory receptors that have delivered them consistent signals. Without an end-target, the nerves can continue to grow to form a thickening of the nerve tissue and send noisy signals back to the brain.
“The most promising therapies involve rethinking how the amputation surgery is actually performed, for instance grafting the nerves into a new muscle or skin, so they have a new home to attach to.”
Of the three participants, one had substantial limb pain prior to amputation but received a complex procedure to graft the nerves to new muscle or skin; she no longer experiences pain. The other two participants, however, received the standard treatment and continue to experience phantom limb pain.
The study suggested that because the brain maps are preserved, it should, in theory, be possible to restore movement to a paralyzed limb or for the brain to control a prosthesis.
“Now that we’ve shown these maps are stable, brain-computer interface technologies can operate under the assumption that the body map remains consistent over time,” said Schone. “This allows us to move into the next frontier: accessing finer details of the hand map—like distinguishing the tip of the finger from the base—and restoring the rich, qualitative aspects of sensation, such as texture, shape, and temperature. This study is a powerful reminder that even after limb loss, the brain holds onto the body, waiting for us to reconnect.”
Editor’s note: This story was adapted from materials provided by the University of Cambridge.
The open-access study, “Stable cortical body maps before and after arm amputation,” was published in Nature Neuroscience.




