A new surgical technique devised by Massachusetts Institute of Technology (MIT) researchers could allow prosthetic limbs to feel more like natural limbs. Through coordination of the patient’s prosthetic limb, existing nerves, and muscle grafts, people with amputations would be able to sense where their limbs are in space and to feel how much force is being applied to them. This type of system could help reduce the rejection rate of prosthetic limbs, which is around 20 percent. The study describing the technique demonstrated in rats was published May 31 in Science Robotics.
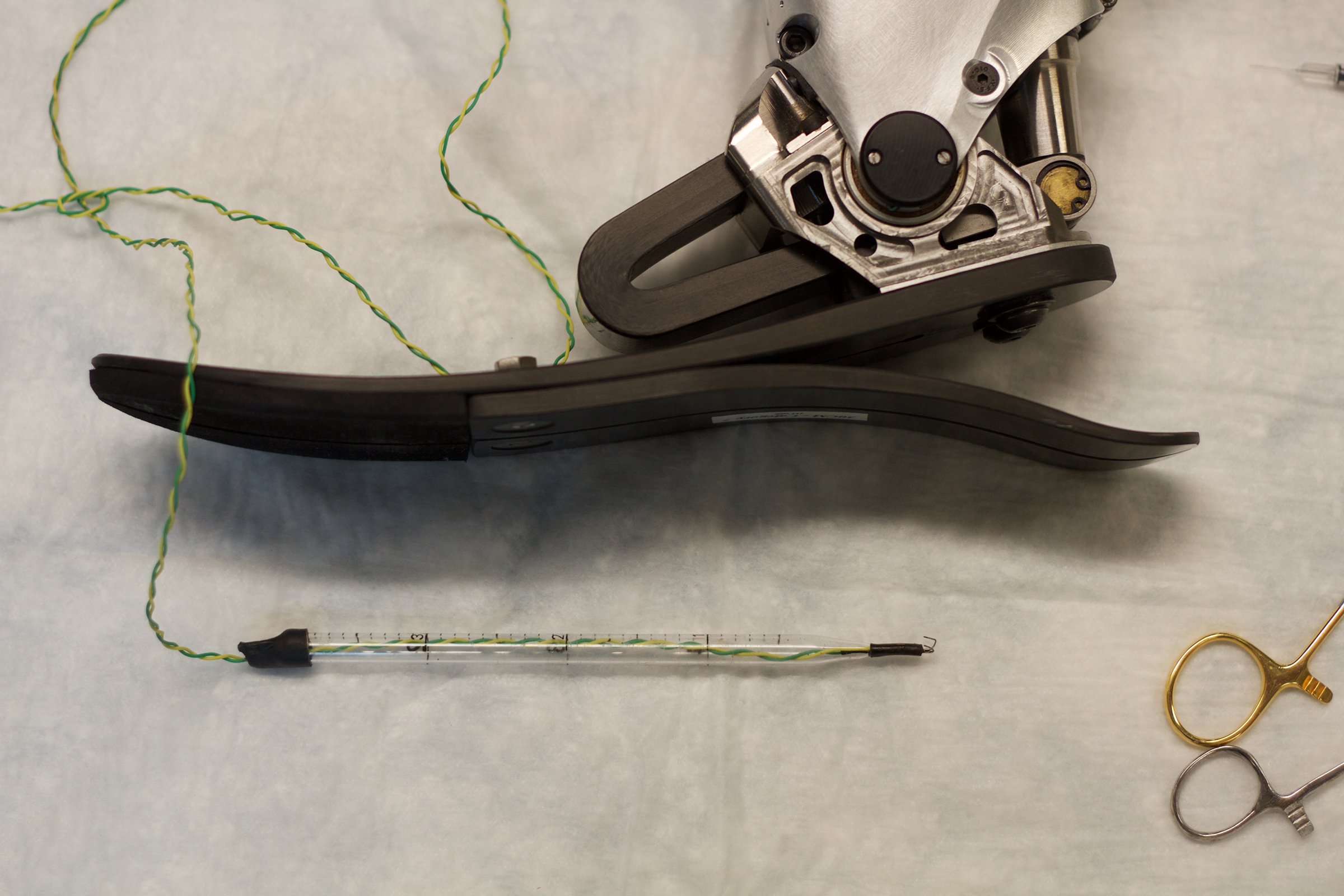
MIT researchers are developing a new surgical approach that would allow people with amputations to receive sensory feedback from their prosthetic limbs and improve their ability to control them. Photograph by Jose-Luis Olivares, courtesy of MIT.
Most muscles that control limb movement occur in agonist-antagonist pairs, such that one muscle stretches when the other contracts. This muscle relationship also allows people to independently control position and stiffness at their limb joints. During a conventional limb amputation, muscles are severed in a way that cuts off this key relationship. Therefore, the patient has no way of sensing where the prosthetic limb is in space or the forces applied to the limb; instead, visual cues must be relied upon.
“There’s no robust neural method for a person with limb amputation to feel proprioceptive positions and forces applied to the prosthesis,” said Hugh Herr, PhD, an associate professor of media arts and sciences who heads the Biomechatronics group at the MIT Media Lab, and the senior author of the study. “Imagine how that would completely hinder one’s ability to move, to successfully balance, or to manipulate objects.”
The MIT team set out to re-create these agonist-antagonist muscle relationships. In many people with amputations, the nerves that send signals to the amputated limb remain intact. The researchers decided to take advantage of those nerves by connecting them to muscle pairs grafted from another part of the body into the amputation site. These grafts, which would be about 4cm by 1.5cm in humans, consist of a pair of muscles that work together like natural muscles. When the brain sends signals instructing a limb to move, one of the grafted muscles will contract, and its agonist will extend. The agonist muscle then sends feedback to the brain about how much the muscle moved and the forces applied to it.
In the Science Robotics paper, the researchers demonstrated in rats that their technique generates muscle-tendon sensory feedback to the nervous system—when the rats contracted one muscle of the pair, the other muscle would move in the opposite way and send sensory information back to the brain—which should be able to convey information about a prosthetic limb’s placement and the forces applied to it. The researchers plan to begin implementing this approach in humans, including Herr, who underwent bilateral transtibial amputations when he was 17.
In other work, the researchers developed a control system that will translate the nerve signals into instructions for moving a microprocessor-controlled prosthetic limb. When the brain sends nerve impulses to the regenerated muscles, those signals will also be received by the microprocessor. Neural stimulations will cause the agonist muscle to contract and the antagonist muscle to stretch. The stretched muscle will then provide neural feedback to allow the patient to feel where his or her limb is in space. The researchers expect that the brain will be able to rapidly learn how much control it must exert to make a prosthetic limb move in the desired way.
“When a patient imagines moving their phantom limb, signals will be sent through nerves to the surgically constructed muscle pairs. Implanted muscle electrodes will then sense these signals for the control of synthetic motors in the external prosthesis,” Herr said.
This type of feedback system should also allow people with a prosthetic arm, for example, to feel a torque applied to the prosthesis. The researchers anticipate this strategy could work for nearly any person with an amputation, including people whose amputations were performed many years ago.
“For almost any amputation scenario, as long as we have a little bit of the healthy nerve left, we can take that and put it into regenerative muscle grafts. We can harvest these muscle grafts from almost anywhere in the body, making this applicable to a large number of cases ranging from trauma to chronic pain,” said Shriya Srinivasan, a graduate student in the Harvard Medical School-MIT Program in Health Sciences and Technology (HST), and the paper’s lead author.
Editor’s note: This story was adapted from materials provided by MIT.




