 |
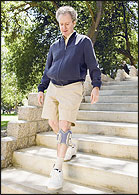
| Photograph courtesy of Bioness Inc. |
FES devices may actually be assisting the brain to recover function through a phenomenon known as neuroplasticity.
Today’s applications of functional electrical stimulation (FES) are fairly recent developments. However, the medical use of electricity goes back to 46 A.D., when the electrical discharges of the torpedo fish were used to treat headache and gout, notes Peter H. Gorman, MD, of the National Institutes of Health (NIH).
With the advent of electrical generators and capacitors in the 18th century, some healthcare practitioners touted the use of electrical charges to cure paralytic disease. Fast forward to today, when the explosion of knowledge in basic and clinical neuroscience has provided rehabilitation medicine with the technology and scientific basis for modern clinical applications of FES.
Even though the incredible advances in high-tech prosthetics for amputees have deservedly captured the media and public spotlight, a “quiet revolution” has been occurring in orthotics with the use of FES. Arguably, the best-known current use of FES is as one aspect of complex multiple strategies, research, and clinical applications involved in treating spinal cord injury (SCI). In the O&P profession, however, drop foot treatment is the major focus for the use of FES.
Electrical stimulation offers benefits in two different areas: function (FES) and therapeutic (TES). Other terms associated with the modality include functional neuromuscular stimulation (FNS) and neuromuscular electrical stimulation (NMES).
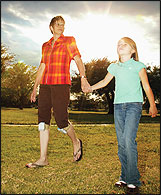 |
| Photograph courtesy of Innovative Neurotronics. |
Drop foot can result from upper motor neuron injuries such as stroke, traumatic brain injury (TBI), multiple sclerosis (MS), and incomplete SCI. The person is unable to raise and lower his foot and ankle, which makes walking a challenge. The patient may drag his foot and toes or try to clear his foot by overcompensating with a high-stepping motion or swinging the leg out to the side and raising the hip to clear distance for the foot.
Devices have been developed to electrically stimulate the dorsiflexor muscles of the foot during the swing phase of gait to provide toe clearance and thus an easier, more natural gait, as well as increased stability, independence, and confidence in walking. These include the L300TM from Bioness Inc., Valencia, California; the WalkAide® from Innovative Neurotronics, Bethesda, Maryland; and the FreeStepTM from Bioflex Inc., Columbus, Ohio.
Bioness is one of the companies founded by famed billionaire entrepreneur and philanthropist Alfred Mann, who has donated millions to universities for research and focused on devices to aid persons with disabilities. Innovative Neurotronics is a wholly owned subsidiary of Hanger Orthopedic Group.
These FES devices are likely only the harbingers of a broader range of orthotic clinical applications to come. Innovative Neurotronics and Bioness are looking to new product developments, and indications are that other companies may be entering FES devices in the O&P marketplace.
These devices, along with others, have been termed neuroprosthetics. Although prosthetics is generally associated with replacing missing limbs, neuroprosthetics involves replacing a missing brain function, explains Innovative Neurotronics President Jeff Martin. Speaking about the WalkAide, Martin says it’s like “a brain in a box” for replacing absent brain signals for gait function. Besides facilitating more normal gait motion, these devices can decrease muscle atrophy from disuse, increase local blood circulation, reduce spasticity, and increase joint range of motion.
Patients with drop foot secondary to upper motor neuron lesions from stroke, MS, cerebral palsy (CP), incomplete SCI, or TBI may be able to benefit from these FES devices, according to Helen Rogers, PT, PhD, who was previously on the faculty of the University of Texas Medical Branch at Galveston (UTMB) before joining Innovative Neurotronics.
Regaining Function through Neuroplasticity?
One fascinating aspect of these FES devices is that they may actually be assisting the brain to recover function through a phenomenon known as neuroplasticity, the brain’s ability to reorganize itself by forming new neural connections. Neuroplasticity occurs under two primary conditions: normal brain development; and as an adaptive mechanism to compensate for lost function and/or to maximize remaining functions in the event of brain injury.
 |
| Photograph courtesy of Bioness Inc. |
Commonly, these rearrangements involve changes in the connection between linked neurons in the brain. In the case of damage, brain reorganization takes place by mechanisms such as axonal sprouting, where undamaged axons grow new nerve endings to reconnect neurons with previous severed links. Undamaged axons also can sprout nerve endings and connect with other undamaged nerve cells, thus making new links and neural pathways. For example, although each brain hemisphere has its own tasks, if one brain hemisphere is damaged, the intact hemisphere can sometimes take over some of the functions of the damaged one.
New connections can form at an amazing speed, but research has shown that neurons need to be stimulated through activity to make these connections, thus aiding rehabilitation.
Some FES devices, including those previously mentioned, are thought to assist in this process.
Kevin Scribner, CO:
|
“Cortical reorganization, or neuroplasticity, is something we all believe in but is difficult to prove at this point,” says Todd Cushman, vice president of business development for Bioness. “We know that the brain is doing something to address deficit because people who have suffered strokes with no change in condition for three or four years apply electrical stimulation and have a positive change in their condition.” In some cases, these changes have continued even when the device is not in use.
“There’s no question that consensus is developing that neuroplasticity plays a large part,” says Martin, citing a research study participant who had suffered a stroke and who regained mobility that was believed to be permanently lost (“Peroneal Nerve Stimulation versus an Ankle Foot Orthosis for Correction of Footdrop in Stroke: Impact on Functional Ambulation,” Lynne R. Sheffler, Maureen T. Hennessey, Gregory G. Naples, and John Chae. Neurorehabilitation and Neural Repair, September 2006).
“There seems to be a positive neuroplastic effect from long-term use of the WA2 [WalkAide],” according to a research study titled “Clinical Perspectives in Fitting the WalkAide2 Foot-Drop Stimulator,” by Jenny Robertson, BScR, and Maura Whittaker, BScR, both of the G. F. Strong Rehabilitation Centre, Vancouver, Canada. The study was presented during the Tenth Annual Conference of the International FES Society in 2005. “This has been shown in other studies on FES and needs further study in subjects who regularly use peroneal nerve stimulation for walking.”
Research Results Promising
Research studies on FES have shown positive results in regard to gait enhancement.
“With the considerable progress made in recent years in the development of FES devices to enhance gait, it appears the clinician is playing an increasing role in the assessment and selection of hemiparetic individuals who might benefit from this technology,” note Robertson and Whittaker. “Technology may have more widespread application if therapeutic considerations are a fundamental part of the assessment process.” The researchers note that the application of the WalkAide technology was enhanced with careful clinical assessment and a possible prescription of an FES exercise regimen. An AFO can be combined with stimulation when stability at the ankle and improved heel strike are required. “Adjunct therapy administered prior to programming the WA2 appeared to facilitate better outcomes,” the researchers say. “Without a full clinical assessment, candidates who could benefit from this technology might be overlooked.”
The 2006 study in Neurorehabilitation and Neural Repair indicates that stroke patients may continue to improve past the traditional 12-week period beyond which further functional gain was considered unlikely. At the three-month mark, the walking speed of patients wearing the WalkAide increased by 15 percent. With continued use of the WalkAide system through six months, the patients’ walking speed increased by 32 percent. Even more encouraging, after 12 months, the patients’ walking speed increased by nearly 50 percent. The study also shows the number of steps taken per day increased significantly over the year. Patients suffering from drop foot due to SCI, TBI, and other pathologies such as MS and CP were included in the study and also experienced the same positive results.
A clinical trial of WalkAide currently under way is focusing on patients who have suffered a stroke within the past year, says Conrad Kufta, MD, former senior staff neurosurgeon in the Surgical Neurology Branch of the NIH and now chief medical officer for Innovative Neurotronics. The multicenter research study involves major medical centers including Washington University School of Medicine and Barnes-Jewish Hospital in St. Louis, Missouri; University of Pittsburgh Medical Center, Pennsylvania; The Institute for Rehabilitation and Research (TIRR), Houston, Texas; and the University of California, San Francisco; among others.
Regarding the Bioness L300, a study titled “Effects of a New Radio Frequency-Controlled Neuroprosthesis on Gait Symmetry and Rhythmicity in Patients with Chronic Paresis,” by J.M. Hausdorr and H. Ring, published this year in the American Journal of Physical Medicine & Rehabilitation, concludes, “The studied neuroprosthesis enhances gait and improves dynamic stability in chronic hemiparetic patients, supporting the idea that this is a viable treatment option in the rehabilitation of patients with foot drop.”
Contraindications
While this research is promising, the manufacturers agree that these devices are not for everyone.
Contraindications include recent surgery near or at the site of stimulation; epilepsy; use of certain types of pacemakers and implants; fractures, dislocations, or cancer in the leg; sciatica; peripheral neuropathy; lumbar spinal stenosis; post-polio syndrome; heart disease; or Guillain-Barre syndrome, according to the companies.
How Are Devices Working in the ‘Real World’?
Some O&P clinicians have posted references to the WalkAide on the OANDP-L listserv noting success with patients using the device. One commented that he has fitted five WalkAide units over the past year for stroke and MS patients and that the devices had made a dramatic difference. All had been AFO wearers previously. The WalkAide was described in a couple of posts as having “awesome potential” and being “the future of orthotics.”
Some comments note the learning curve involved in customizing and fitting the devices and express concerns about reimbursements from third-party payers. However, the manufacturers note that many private insurance companies and workers compensation plans will cover the device. Efforts are under way to obtain Medicare coverage.
For both clinicians and patients, one of the most exciting aspects of these FES devices is seeing instant improvement. “You can see it work right away,” says Cushman. “It’s immediate gratification.”
Some information for this article was adapted from information on the Stanford University website: www.stanford.edu. Device descriptions can be found below.
Miki Fairley is a contributing editor for The O&P EDGE and a freelance writer based in southwest Colorado. She can be contacted via e-mail at [email protected]
Editor’s note: The O&P EDGE does not endorse any company or product. Companies and products mentioned in this article are for reader information only. This article may not provide complete coverage of available FES devices with orthotic or prosthetic application.
A Closer Look at FES Devices
|






