Diminishing Returns
 |
| John W. Michael, C.P.O. |
It’s not just O&P. All healthcare fields have
been impacted by a manpower shortage with regard to recent
recruitment-not because there aren’t talented minds and
skilled hands out there; not because O&P and other healthcare
professions don’t have the charisma to attract them-but
because reimbursement problems have become so prevalent since the
rise of managed care. Knowledge of this situation has percolated
beyond O&P, as well as healthcare in general, and has
discouraged candidates who might otherwise consider O&P as
their life’s work, believes John Michael, CPO, noted clinician and
consultant.
“There are certainly a smaller number of people interested in
coming into the O&P field,” says Michael. Every facet of
healthcare has been affected by managed care-and many of them
have been hit harder than the O&P field, Michael says, pointing
out that physician recruitment is down between 30 and 40 percent.
Therapists and nurses have declined too. “The whole system has been
disrupted,” Michael points out. “Why would a young person choose to
enter the O&P field and face the reimbursement hassles?”
As long as the government continues to tamper with
reimbursements and encourage managed care, most people will choose
a career that is more stable and more lucrative than healthcare,
Michael says, adding, “We lose a good chunk of students who are
well-qualified, but did the expedient thing.
“On the other side of the coin, I’m impressed with the quality
of the people who are coming into the field, undaunted by the
financial aspect-good folks who genuinely want to help
patients and are willing to get their hands dirty.”
Reimbursement: Continuing Influence
How might the reimbursement picture continue to influence
recruitment of potential O&P professionals?
A study by Caroline Nielsen, “Issues Affecting the Future Demand
for Orthotists and Prosthetists: Update 2002,” published in July,
concludes that:
• Reimbursement for technologically advanced products will
be increasingly dependent on demonstrating improved quality of life
and long term cost-effectiveness;• Without continuing improvements in reimbursement
policies, an increasing number of persons are likely to be paying
for orthotic/prosthetic products from their own resources;• An increase in the number of insurers requiring patient
care to be provided by an orthotist/prosthetist certified by the
American Board for Certification in Orthotics and Prosthetics (ABC)
would increase the share of the market and the number of certified
practitioners required to meet patient needs; and• In this fluctuating reimbursement environment, research,
public relations, and educational efforts are essential to
demonstrate the high quality and cost-effectiveness of patient care
by certified orthotists/prosthetists.
The demographics picture presents both challenges and
opportunities for the future of O&P.
Robin Seabrook, executive director of the National Commission on
Orthotic and Prosthetics Education (NCOPE) points to findings
highlighted in Nielsen’s newly updated study:
• By 2010 the baby boom population will be between the
ages of 46-64, creating a rapid increase in the proportion of the
population at highest risk for those diseases/disabilities
requiring orthotic/prosthetic care. A dramatic increase in the
older age groups after the year 2015, due to the aging baby
boomers, will significantly increase the demand for both orthotists
and prosthetists;• The number of persons using orthoses is expected to
increase by at least 31 percent by the year 2020. Without an
increase in graduates, the projected number of orthotists available
in the year 2010 will be able to serve only 61 percent or less of
the population using orthoses;• The total number of persons with an amputation is
expected to increase by at least 47 percent by the year 2020.
Without an increase in graduates, the projected number of
prosthetists available in the year 2010 will be able to serve only
66 percent or less of the population using prostheses. With a 10
percent increase in graduates in the year 2010 and another 10
percent increase in 2015, the projected number of prosthetists
available in 2020 will still be able to serve only 66 percent of
the population using prostheses.
O&P Schools: What’s the Prognosis?
Like the wetlands, are O&P programs and schools vanishing?
Do they need federal funding to protect and preserve them? If they
disappear, where will tomorrow’s practitioners be trained?
Seabrook agrees that there has been a decline in
enrollment in O&P schools and programs over the last three to
four years: “It’s not statistically significant, but any decrease
at all in a field as small as ours can be regarded as
significant.”
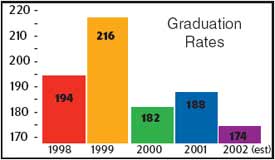
Graduation rates for the eight baccalaureate and certificate
programs in the seven schools accredited by the Commission on
Accreditation of Allied Health Education Programs (CAAHEP) and
NCOPE vary from 194 in 1998 to 216 in 1999, 182 in 2000, 188 in
2001, and a projected 174 in 2002, Seabrook reports.(Four schools
also provide accredited technician programs.) Despite the clear
need for more and expanded programs, Seabrook notes that attempts
to establish O&P masters programs have had poor success rates:
“One masters program-in Iowa-folded before it even
started.”
However, the future appears brighter, Seabrook points out, as
the Georgia Institute of Technology, Atlanta, is currently
implementing its masters program and accepting the first students
this fall. [Editor’s note: For more information on Georgia Tech’s
masters program, visit www.ap.gatech.edu/mspo] .
 |
| Mark Edwards, CP |
Northwestern University, Chicago, is also looking
into a master’s level program. “A graduate level education is
necessary,” affirms Mark Edwards, CP, director of Prosthetics
Education at Northwestern. “I don’t know that a graduate degree
will be mandatory, but it is needed to grow the profession from
within, so that we have individuals equipped to become the faculty,
researchers, and leaders of the profession.”
“We certainly need more schools,” believes Morris Gallo, CPO, a
member of the Florida licensure board and one of the architects of
the state’s licensure law. “Classes are very small and not
conveniently spread around the country, and they seem to be always
teetering for lack of funding.” Programs at New York University
(NYU) and the University of California-Los Angeles (UCLA) went
under after 20 years, because there wasn’t enough money to sustain
them, Gallo says. “Diminishing funding was only part of the
problem; there were also legal limits placed on what they could
charge students.
“To me, it’s a national security issue,” Gallo continues.
“Military personnel are coming back wounded, and they have no place
to go. Veterans moving to Florida may not be able to get a
new-patient appointment for O&P services at a VA center for
three years. And without new practitioners entering the field, it’s
only going to get worse.”
 |
| Don Fedder, DrPH |
So where is the future O&P practitioner coming
from? “The future practitioners are going to come from the same
place as they do now,” says Don Fedder, DrPH, president and CEO of
the Board for Orthotist/Prosthetist Certification (BOC). “But it
won’t be from the university base. We’re competing with large
numbers of nurses, pharmacists, and physicians for educational
funding; there’s just no money left over for O&P. So we have to
take the practical approach. I don’t have a crystal ball, but
unless there is some kind of unforeseen intervention that I can’t
imagine, the primary route for those who want to train in this
field will continue to be apprenticeship.
“I’m not opposed to education,” he adds promptly. “As a matter
of fact, five PhDs have graduated under my tutelage. There’s no
question that there is a fundamental scientific and engineering
base that underlies O&P. You’ve got to know something about
gait control; you’ve got to know something about materials; you’ve
got to understand the mechanics of an artificial leg to be able to
align it.
 |
| Ron Manganiello |
“Someone who has been trained in a technical way
can advance to a point where they become extremely skilled and know
exactly what they have to do, and do it,” he continues. “There are
alternate pathways to get to the goal, which is to have a competent
practitioner who can take care of patients.”
Seabrook agrees that, although the reason applications in
O&P programs are down is still “the $10,000 question,”
healthcare career choices today don’t attract as much interest as
other fields providing easier, faster money. The good news, she
said, is that applications are back up to their usual numbers for
the 2003 academic year. “We may be seeing a reemergence of
interest,” she noted hopefully.
Are Gender Surprises in Store?
Will more women practitioners help fill the gap?
 |
| Susan Kapp, CPO |
“I am proud to report that about 40 percent of the
patient care practitioners at New England Orthotic & Prosthetic
Systems are women,” says Ron Manganiello, CEO. “We currently have
22 practitioners, of whom eight are women. It is also interesting
to note that three of our women practitioners are branch office
managers/partners. We are also currently negotiating with two
additional certified women practitioners that we haven’t yet hired.
As far as I know, we have the highest percentage of women
practitioners of any O&P company around.
“We haven’t targeted women in particular. But for whatever
reason-or perhaps simply by coincidence-we are seeing
many women practitioners right now, who are either in our markets
competing with us, or looking for jobs, or recruiting. I think it’s
a great field for women to enter.”
Susan Kapp, CPO, assistant professor and director, University of
Texas Southwestern Prosthetics-Orthotics Program, Dallas, notes
that about one-third of Southwestern’s O&P classes are females;
NCOPE’s June 2002 quarterly newsletter reports that 21 percent of
597 graduates completing residencies through NCOPE programs since
1995 were female.
Judith Otto is a freelance writer based in Holly Springs, Mississippi.