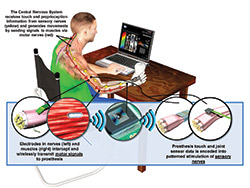
DARPA’s HAPTIX program aims to develop fully implantable, modular, and reconfigurable neural-interface systems that would enable intuitive, dexterous control of advanced upper-limb prosthetic devices. Image courtesy of DARPA.
The Defense Advanced Research Projects Agency (DARPA) announced that it has awarded prime contracts for Phase 1 of its Hand Proprioception and Touch Interfaces (HAPTIX) program to create a prosthetic hand system that moves and provides sensation like a natural hand. DARPA is working with teams led by Case Western Reserve University (CWRU); Cleveland Clinic; Draper Laboratory, Cambridge, Massachusetts; Nerves, Dallas; Ripple, Salt Lake City, University of Pittsburgh (Pitt); University of Utah (U of U); and University of Florida.
HAPTIX seeks to create a prosthetic hand system that moves and provides sensation like a natural hand such that it creates a sensory experience so rich and vibrant that users would want to wear their prostheses full time. By restoring sensory functions, HAPTIX also aims to reduce or eliminate phantom limb pain, which affects about 80 percent of amputees. The program plans to adapt one of the prosthetic limb systems developed recently under DARPA’s Revolutionizing Prosthetics (RP) program to incorporate interfaces that provide intuitive control and sensory feedback to users. These interfaces would build on advanced neural-interface technologies being developed through DARPA’s Reliable Neural-Interface Technology (RE-NET) program.
“The ultimate goal for HAPTIX is to create a device that is safe, effective, and reliable enough for use in everyday activities,” said Doug Weber, PhD, DARPA program manager.
DARPA is evaluating several distinct technical approaches in Phase 1. Those that prove successful will continue into Phase 2, which will integrate selected technology components into a complete HAPTIX test system. The agency plans to initiate take-home trials of a complete, U.S. Food and Drug Administration-approved HAPTIX prosthesis system within four years.
Where appropriate, HAPTIX teams intend to leverage commercially available technologies such as intramuscular electrodes and lead technologies developed initially for cardiac pacemakers that are now used in several modern implantable medical devices. The program also plans to test advanced microelectrode array and nerve cuff electrode technologies that have been developed over the past two decades with support from the National Institutes of Health, the U.S. Department of Veterans Affairs, and DARPA. To help the Phase 1 contractors conduct their research more quickly and cost effectively, DARPA is providing prosthetics simulation software for testing designs.
HAPTIX Phase 1 contract awardees have also received grants to advance their work:
- CWRU: A team led by associate professor of biomedical engineering Dustin Tyler, PhD, received $4.4 million to test high-density electrode nerve cuffs to stimulate nerves in the residual limb directly above a prosthetic arm so that a user can control the prosthesis more naturally and also experience sensation. The cuffs wrap around major nerves in the arms or legs and stimulate them electrically, which results in muscle contraction and simple movements.
- Cleveland Clinic: A team led by Paul Marasco, PhD, was awarded a $2.5 million contract to use cutting-edge science to develop a suite of clinically relevant outcome metrics to evaluate advanced prosthetic limb technology. “These advances could help physicians make better clinical care decisions, justify to payers the need for advanced prosthetic devices, and ultimately improve the quality of life for persons with upper-limb amputations,” Marasco said.
- Nerves: A team led by neurophysiologist and engineer Edward Keefer, PhD, will develop algorithms for translating neural signals that control motion in a manner such that they convey information to the nerves that interact with an implanted interface system. The grant amount has not been disclosed. A team led by John M. Miguelez, CP, FAAOP, with Advanced Arm Dynamics (AAD), Redondo Beach, California, will work with the Nerves team on implantable peripheral nerve control of electric prostheses. AAD will provide patients, prosthetic fitting and testing, and therapeutic training with standardized outcome measures to establish the patients’ baseline status and provide a means to quantify change in the patients’ prosthetic function.
- Ripple: Director of Research Daniel McDonnall, PhD, and his colleagues have developed a wireless device to be implanted directly into muscles that collects information from the muscles and sends that information wirelessly to an external receiver built into the prosthetic limb. The implant should allow users to freely move multiple joints in the prosthetic limb at the same time. The company has received a $5.9 million grant to develop a smaller version of the device that will be used in clinical studies by U of U and Pitt. Chris Lake, CPO, FAAOP, clinical director at Lake Prosthetics and Research, Euless, Texas, will provide clinical prosthetic consulting to Ripple.
- Pitt: Robert Gaunt, PhD, an assistant professor, and his co-director Michael Boninger, MD, a professor and chair, both with the Pitt School of Medicine Department of Physical Medicine and Rehabilitation, have received funding in an undisclosed amount to lead a multidisciplinary research team that will recruit five volunteers to try to demonstrate that stimulation of the sensory portion of the spinal cord nerves, which would normally innervate the hand and forearm, can cause an individual with an amputation to feel distinct sensations of touch and joint movement in the “phantom” hand and wrist. They also plan to insert fine-wire electrodes into the forearm muscles of able-bodied volunteers to collect and interpret muscle signals to guide movement of a virtual prosthetic hand to control hand opening and closing, as well as thumb movement. Eventually, the team aims to devise a fully implantable system for home use.
- U of U: Bioengineering associate professor Gregory Clark, PhD, is leading a research team that received a $1.4 million grant to further develop an implantable neural interface that will allow an individual with an upper-limb amputation to move an advanced prosthetic hand with just his or her thoughts, and to pay for testing on two human volunteers. The device, called the Utah Slanted Electrode Array, was developed by Richard A. Normann, PhD. It uses 100 electrodes that connect with nerves in the residual arm to read signals from the brain telling the hand how to move. Likewise, the neural interface delivers meaningful sensations of touch and movement from a prosthetic hand back to the brain. )
- Draper Laboratory and the University of Florida have also been awarded grants. Information about their roles is not yet available.




