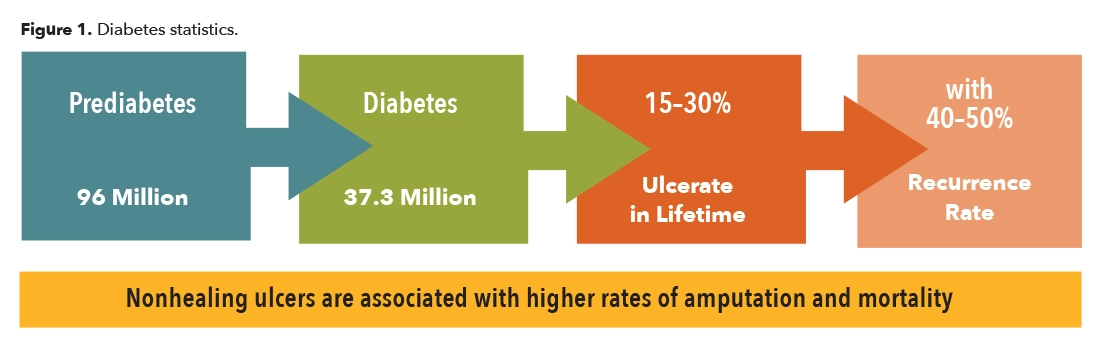
Diabetes mellitus is a disease where the body either does not produce enough insulin or becomes insulin resistant, and there are elevated levels of glucose in the blood stream. With time, high blood sugar has manifold effects including neuropathy due to the deterioration of the peripheral nerves. One of the results is loss of protective sensation. This occurs first where the nerves are finest, in the extremities, leaving them vulnerable to injury and ulceration. Patients with advanced neuropathy often complain of numbness, tingling, or burning in their fingers, hands, toes, or feet. In addition, due to other complications from the disease, when skin breakdown occurs it is slow to heal, taking months or even years. This in turn can begin an expensive cycle of wound infections that may lead to amputation. Diabetes continues to be the number one cause of the approximately 150,000 amputations performed each year in the United States. According to the Centers for Disease Control and Prevention, there are 154,000 hospitalizations associated with diabetic lower-extremity amputations annually, which puts a huge financial burden on the healthcare system (Figure 1).1
Support authors and subscribe to content
This is premium stuff. Subscribe to read the entire article.





