
 Prosthetists and orthotists are responsible for treating the musculoskeletal dysfunction of their patients, although these conditions and disorders commonly involve more than physical symptoms. Treating all patients the same by providing biomechanically successful devices and the same cookie-cutter speech upon evaluation or delivery fails to recognize that each patient has specific needs based on their medical history or personal background. The typical flow of an appointment may be altered when the O&P patient has a cognitive or speech deficit, behavioral impairment, or anxiety brought on by medical environments. Clinicians may shift the conversation to the caregivers or parents, skipping over the patient entirely. Patient-centered care refocuses and modifies the clinician’s role to include the patient, which may mean explaining the same thing in two different ways.
Prosthetists and orthotists are responsible for treating the musculoskeletal dysfunction of their patients, although these conditions and disorders commonly involve more than physical symptoms. Treating all patients the same by providing biomechanically successful devices and the same cookie-cutter speech upon evaluation or delivery fails to recognize that each patient has specific needs based on their medical history or personal background. The typical flow of an appointment may be altered when the O&P patient has a cognitive or speech deficit, behavioral impairment, or anxiety brought on by medical environments. Clinicians may shift the conversation to the caregivers or parents, skipping over the patient entirely. Patient-centered care refocuses and modifies the clinician’s role to include the patient, which may mean explaining the same thing in two different ways.
O&P clinics are primarily set up to accommodate auditory learners. Patients and clinicians typically talk back and forth, discussing treatment plans and answering questions. Patients with speech-language pathologies or cognitive deficits, and the pediatric population may not be capable of participating in this verbal exchange.
Clinicians should attempt to explain the process of the appointment and treatment plan with the patient at the patient’s level of understanding. Implementing visual tools is an easy way to promote patient respect and autonomy by providing information about medical procedures at the appropriate level of comprehension.
Communicating with individuals with intellectual deficits can be viewed as similar to using
a foreign language translator, as both parties do not speak the same language fluently. Implementing visual schedules or pictorial cues can bridge any understanding gap during medical appointments. Patients of all ages with communication, intellectual, or behavioral deficits often get grouped together as a population that cannot understand what is happening to them, or why. To keep appointments moving along, clinicians sometimes deliver their script as usual to the parents or caregivers while performing evaluation or follow-up procedures on the patient, without fully acknowledging the patient him or herself. The patient may not be fully capable of comprehending the biomechanical applications of the brace or different modifications, but there should be a genuine attempt to explain the device at the patient’s level of understanding, such as “This brace is to help you walk better.”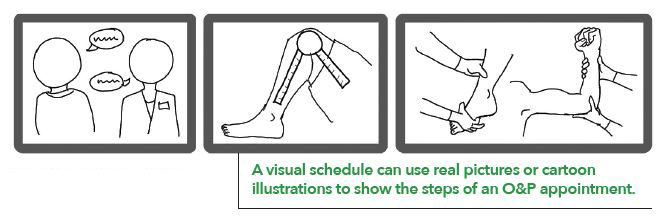
Visual schedules can help explain what is happening, or going to happen, to a patient during an appointment. Studies have found that impairments in social interaction and communication, as well as low cognitive functioning, aggression, anxiety, and other sensory sensitivities contribute to an aversion to medical care.1 Research supports the use of visual aids or picture cues as being an effective technique to teach children with autism at home and at school.1 This principle could be extrapolated to the medical profession and O&P clinics by creating a visual schedule and picture cues for O&P specific situations. The standard of practice, tell-show-do, may be adequate for some patients but is not comprehensive enough to assuage fears and anxiety in others. Nervous patients can make the clinician’s job harder and cause the appointment to run over the time allotted. Looking at dental appointments for children with autism, a study found the addition of a visual schedule system and picture cues allowed the children to successfully complete more steps, progress at a quicker rate, and exhibit lower levels of behavioral distress during the appointment.1
Spending a little extra time at the beginning of the appointment soothing patient anxietiescan save clinicians time and money. This increases the likelihood that patients will feel comfortable and enjoy working with their clinicians, and thus be more willing to participate within an appointment and comply with treatment plans.
A visual schedule can use real pictures or cartoon illustrations to show the steps of an O&P appointment. For a prosthesis or orthosis initial evaluation, the images may include talking to gather patient history, measurements and range of motion, manual muscle testing, and the casting process. Without previous experience, casting a limb is a completely new experience for patients. For patients with cognitive, sensory, or behavioral deficits, casting is a nerve-wracking portion of the appointment and may induce anxiety, thus increasing agitation and muscle tone. Anxiety is frequently a manifestation of fear of the unknown, and can reduce the quality of the casts and subsequent devices created.
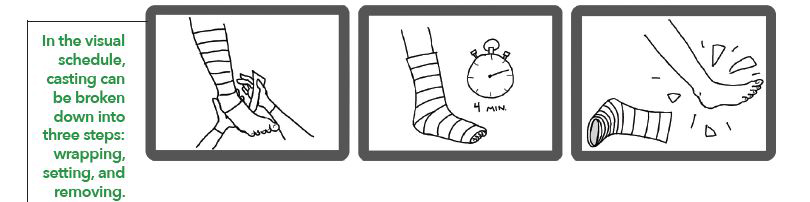
In the visual schedule, casting can be broken down into three steps: wrapping, setting, and removing. This allows patients to be fully aware of what is going to happen, and they can track their progress throughout the procedure. The last step depicts a patient’s limb as once again free. Fear and panic experienced by many patients sets in when the cast begins to harden, and it can be relieved by reminding patients of the “foot free” step coming up next on the visual schedule. The visual aid can be delivered during clinicians’ verbal description of the procedure and used as a reminder throughout the appointment. A visual schedule that patients can see before the procedure starts and follow along throughout the duration of the procedure can be the difference of recasting or remaking a device.
Visual schedules and cues can be implemented into many facets of O&P care. They’re useful for all appointment types and devices in clinic, can be handed out as at-home literature, to show wear schedules, and explain cleaning and maintenance. Picture cue cards can be one-card requests and can help when asking a patient to sit, stand, or walk, etc. Visual tools can also be generated to help teach patients wear schedules or how to don and doff their devices independently. The literature sent home with patients is frequently a dense book from the manufacturer, and many patients would benefit from a simplified version that includes more visual elements. These visual tools can be generated in-house with very rudimentary art skills or by taking pictures, a ubiquitous ability since nearly everyone owns a smartphone. Implementing visual schedules and picture cues is mutually beneficial for the clinician and patient. By receiving information about their medical care in a way they can comprehend, patients’ anxieties and maladaptive behaviors are reduced, which in turn allows clinicians to perform their job to the best of their abilities. O&P EDGE
Emma Newland, MSPO, has a master’s degree in O&P from the University of Pittsburgh and a bachelor’s degree in
neuroscience. She is an orthotics resident at the University of California San Francisco and has extensive experience working with children with speech-language delays and disorders.
Academy Society Spotlight is a presentation of clinical content by the Societies of the Academy in partnership with The O&P EDGE.
References
- Mah, Janet WT, and P. Tsang. 2016. Visual Schedule System in Dental Care for Patients with Autism: A Pilot Study. Journal of Clinical Pediatric Dentistry 40(5):393-9.





