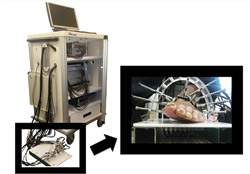
Dynamic diffuse optical tomography system and the measurement probe. Photograph courtesy of Biomedical Optics Express.
People with diabetes are at a higher risk of developing peripheral artery disease (PAD), and individuals with PAD are four to five times more likely to have a heart attack or stroke, according to the American Heart Association. A new optical diagnostic tool, created by Columbia University, New York, New York, researchers and reported in the August 30 issue of Optical Society’s (OSA) open-access journal Biomedical Optics Express, may soon make it easier to diagnose and monitor PAD. This new, noninvasive imaging technique-known as dynamic diffuse optical tomography imaging (DDOT)-uses near-infrared light to map the concentration of hemoglobin in the body’s tissue. This mapping can reveal how effectively blood is flowing to patients’ hands and feet and thus lead to appropriate intervention, which could ward off the occurrence of ulcers that might lead to amputation.
“Currently, there are no good methods to assess and monitor PAD in diabetic patients,” said Andreas Hielscher, PhD, interim chair, professor of biomedical engineering, radiology, and electrical engineering, and director of the Biophotonics and Optical Radiology Laboratory at Columbia, in an OSA press release.
“Patients with PAD experience foot pain, called ‘claudication,’ while walking,” Gautam Shrikhande, MD, assistant professor of clinical surgery, and director of the Vascular Laboratory at Columbia’s Medical Center, was quoted as saying. “This pain continues, even at rest, as the disease progresses. In more advanced stages, PAD patients develop sores or ulcers that won’t heal. Then, cell death, a.k.a. ‘gangrene,’ occurs and amputation is often the only solution. It’s extremely important to diagnose PAD early, because medication and lifestyle changes can alleviate the disease.”
This is where DDOT can help. The instrumentation can provide fast image acquisition and allows for blood volume to be observed over time in response to stimulus such as a pressure cuff occlusion or blockage. It can also provide maps of blood constituents and total hemoglobin concentration throughout the foot and identify regions that require intervention.
To map and monitor the presence of hemoglobin, the protein that carries oxygen in the blood, red and near-infrared light is shone at different angles around areas that are susceptible to PAD. These specific wavelengths of light are then absorbed or scattered, depending on the concentration of hemoglobin. Optical imaging techniques can non-invasively measure blood in tissue without the need for contrast agents or ionizing radiation. Contrast agents pose the risk of renal failure, which is a concern in individuals with diabetes, according to the report.
The report concludes that the preliminary results show that DDOT has the potential to aid in the diagnosis and monitoring of PAD, and it has the potential to fill the diagnostic gap that currently exists within the population of patients with diabetes.
Khalil, Hielscher, and colleagues hope to bring their diagnostic tool to market and into clinics within the next three years.
Editor’s note: This story was adapted from materials provided by the Optical Society and its open-access journal Biomedical Optics Express.




