 In 1980, a Hmong family relocated from Laos to Merced, California, a city about two and a half hours southeast of San Francisco. The youngest child, Lia, began having seizures when she was three months old and was eventually diagnosed with epilepsy. Over a period of several years, differing opinions about her condition and care resulted in repeated conflicts between her parents and the medical staff at the local hospital. In 1988, Anne Fadiman began to research the story and in 1997 published the book The Spirit Catches You and You Fall Down: A Hmong Child, Her American Doctors, and the Collision of Two Cultures. The title of the book comes from the term used in the Hmong language to describe what was happening to Lia when she experienced a seizure.1
In 1980, a Hmong family relocated from Laos to Merced, California, a city about two and a half hours southeast of San Francisco. The youngest child, Lia, began having seizures when she was three months old and was eventually diagnosed with epilepsy. Over a period of several years, differing opinions about her condition and care resulted in repeated conflicts between her parents and the medical staff at the local hospital. In 1988, Anne Fadiman began to research the story and in 1997 published the book The Spirit Catches You and You Fall Down: A Hmong Child, Her American Doctors, and the Collision of Two Cultures. The title of the book comes from the term used in the Hmong language to describe what was happening to Lia when she experienced a seizure.1
Evaluating extreme cases can bring clarity to challenges that we encounter in a more nuanced fashion in everyday practice. In this story of extreme cultural differences, the author does a masterful job of conveying the tension between cultures while telling a sad and frustrating story about a medical condition that seems impossible to manage. A few paragraphs summarizing the book cannot do justice to Fadiman’s in-depth and deeply personal account of the clash between the Lee family and the professionals responsible for Lia’s medical care. The book describes this cultural collision with chapters about the experiences of the Lee family, Lia’s medical care, the perspectives of the medical practitioners directly involved, and explanations of the history and culture of the Hmong people and their experiences in the United States.
Throughout the book, the author presents each side fairly, and demonstrates empathy and sensitivity to each perspective. Fadiman sees this story as challenging our notions of what it means to be a good parent and a good doctor, and what happens when those values collide. Lia’s condition and the challenges created by the collision of values had no simple solution, and Fadiman steers clear of trying to assess blame for the outcome. This article describes the importance of recognizing and affirming cultural differences in healthcare encounters, as well as a strategy for navigating encounters where these cultural differences can impact care and outcomes.
Compliance, or Something Bigger?
Much of the tension in this story relates to the Lee family’s failure to comply with the treatment plan established by Lia’s physicians. In particular, their inability to maintain the rigorous medication schedule required to manage Lia’s frequent seizures resulted in serious medical complications and put Lia’s life at risk. To ensure that the treatment plan was followed, Lia was eventually removed from her parents’ care and placed in foster care. There were many challenges in managing Lia’s seizures, including the large number of medications that had to be taken on a specific schedule, and that her physicians frequently made changes to this regimen in attempts to manage her symptoms most effectively. This complicated medication regimen was especially challenging for Lia’s parents, who were unable to speak English and lacked even a rudimentary understanding of modern medicine. Additionally, professional medical translation services were not readily available, which left hospital staff and home health providers with limited options for communicating complex instructions. The heroic, and ultimately unsuccessful, efforts of numerous allied health providers to overcome these barriers are described in detail in the book.
Language, however, was not the most significant barrier to compliance. Even when the Lee family understood the physicians’ instructions, their view of Lia’s condition kept them from adhering to them. The Lees simply did not agree with Lia’s physicians about the causes and solutions to the child’s problems. As implied by the phrase used by the Hmong people to describe epilepsy, in that culture Lia’s condition was believed to have spiritual roots. Additionally, Lia’s parents believed that the solution to any medical complication she encountered involved using a combination of modern medicine and spiritual intervention. Her parents believed the medication schedule was excessive. Even when they understood the dosage and timing prescribed by her physicians, her parents would modify the amounts to what they considered a more reasonable level.
As medical professionals, we tend to understand compliance simply as a matter of patients following instructions. Patients can only follow instructions they understand, so we need to recognize that different instructional approaches are often required to ensure that information is accurately communicated and understood. Additionally, we must be willing to think about compliance at a deeper level and recognize that adherence requires agreement. A patient or caretaker must agree with the provider about the nature of a problem and the solution before he or she can be expected to follow through on instructions for treatment. Patients are more likely to adhere to what has been agreed to as part of a shared decision-making process. Cultural difference can complicate the process toward agreement, since the parties involved often come from different belief and value systems.
When discussing these dynamics, Fadiman references the work of Arthur Kleinman, MD, a psychiatrist and a professor of medical anthropology and cross-cultural psychiatry at Harvard University. In a 1978 article titled “Culture, Illness, and Care,” Kleinman et al. describe factors related to “the cultural construction of clinical reality,” which can help us understand the importance of culture in medical decision making.2
Disease Versus Illness
Understanding the difference between disease and illness is an important part of navigating cultural differences in the context of medical care. Kleinman describes both disease and illness as explanatory models of sickness, which is a more complex and fluid concept. Modern medicine addresses “abnormalities in the structure and function of body organs and systems,” while illness describes “the human experience of sickness….” When patients suffer illnesses they “experience a disvalued change in states of being and in social function.”2 As an example, prosthetists may see amputation primarily as the end result of a circulatory problem and recommend specific structural replacements for the missing body segment. Patients, on the other hand, may see the same phenomenon primarily in terms of how it disrupts their vocational, avocational, and social capabilities, and how the services of a prosthetist can restore those capabilities. Kleinman et al. could have been describing the collision between the Lee family and Lia’s physicians when stating: “…the remedies prescribed by physicians may fail to cure disease, despite effective pharmacologic action, when patients fail to follow through on the medical regimen because they do not understand (or do not agree with) the physicians’ stated rationale for their actions.”2 Understanding how patients experience sickness is vital to helping them make decisions about how to address it.
Explanatory Models
People from different cultural backgrounds have different frameworks for perceiving reality. It is important to understand how these perspectives impact their understanding of health and medical care. “Clinical realities are…culturally constituted,” and the basis for many decisions related to medical care, such as when and where to seek it, its duration, and how to evaluate whether it has been successful, come from outside the culture of biomedicine.2 Kleinman describes all medical encounters as “transactions between explanatory models” that often involve “major discrepancies in cognitive content, as well as therapeutic values, expectations, and goals.…”2 Rather than give instructions and expect patients to follow them, healthcare providers must understand how patients understand their own illness and disease, and negotiate a treatment plan that takes those views into consideration. Cultural collisions occur, in part, because within the biomedical culture we assume that “biological concerns are more basic, ‘real,’ clinically significant, and interesting than psychologic and sociocultural issues. Disease, not illness, is the chief concern; curing, not healing, is the chief objective.”2 This perspective “emphasizes a technical ‘fix’ rather than psychosocial management. It is less concerned with ‘meaning’ than other forms of clinical care. It deals with the patient as a machine.”2 A reorientation of our perspective and approach to account for the psychosocial factors that often play a larger role in our patients’ understanding of sickness and health can improve the effectiveness of the biomedical solutions we offer. Approaches that do not consider the patients’ views of their illnesses can contribute to noncompliance, dissatisfaction, and suboptimal care.
A lack of understanding and agreement is more likely when patients come from a broader culture that views illness outside of the biomedical framework. It is especially important in these encounters for the practitioner to understand the patient’s perspective. “Comparison of [the] patient model with the doctor’s model enables the clinician to identify major discrepancies that may cause problems for clinical management. Such comparisons also help the clinician know which aspects of his explanatory model need clearer exposition to patients (and families), and what sort of patient education is most appropriate.”2 In other words, even if we remain convinced of the superiority of biomedical explanations and solutions, understanding the patient’s perspective allows us to focus our education efforts in a way that is most likely to resonate with the patient. Kleinman suggests asking the patient and family members a series of questions that are designed to help in this regard. (See Eight Questions.)
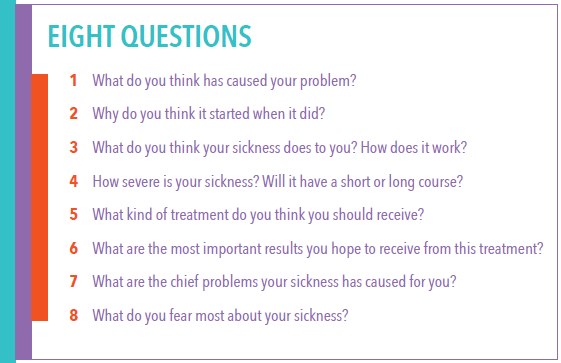
Kleinman’s work focuses on providing medical care across significant cultural divides, but explanatory models can vary significantly even within ethnic groups, geographical areas, and family systems, and “reflect social class, cultural beliefs, education, occupation, religious affiliation, and past experience with illness and healthcare.”2 Namratha Kandula, MD, a professor of medicine at Northwestern University, believes that “asking about the patient’s explanatory model should be used with all patients, and in routine clinical encounters—because the vast majority of patients are not from the culture of biomedicine.”3 Kandula simplified Kleinman’s questions to two, which she asks whenever seeing a new patient: “‘How is your health?” followed by, ‘How do you know?'”3
Explanatory Models in P&O
Many of the medical problems that we encounter in O&P practice are not as challenging as those that Lia Lee presented with. In many cases, the problem can be easily identified, and our intervention makes a dramatic enough improvement in mobility and quality of life that it is unlikely to be challenged on cultural grounds. But what about the situations when things are not so clear and outcomes not so dramatic? Our interventions do not cure chronic conditions, and those conditions often take an increasing toll on those we work with. In the case of congenital conditions with no cure, or chronic, progressive conditions, our job is often to mitigate the effects of the condition and help patients maintain as much quality of life as is possible while their overall health deteriorates. These challenges can complicate shared decision making, since much more is at stake than the patients’ immediate structural or mobility needs. In these situations, making decisions about what course of treatment to pursue and how to design the intervention requires additional sensitivity to what patients and caretakers value.
Working with individuals from a different culture can be a rewarding experience. Fadiman describes ways in which the Hmong culture enriched her understanding of family, support, and caring. We can miss these valuable perspectives when focused exclusively on providing biomedical solutions. Modern medicine offers tangible solutions to disease problems, and Kleinman points out that “only modern health professionals are potentially capable of treating both disease and illness.”2 Our efforts to offer these solutions to individuals from different cultures will be more successful if we learn to acknowledge their perspectives and develop skills necessary to incorporate them into the decision-making process. Our own lives will be enriched as we open ourselves up to perspectives that are different from our own.
John T. Brinkmann, MA, CPO/L, FAAOP(D), is an assistant professor at Northwestern University Prosthetics-Orthotics Center. He has more than 20 years of experience treating a wide variety of patients.
References
Support authors and subscribe to content
This is premium stuff. Subscribe to read the entire article.




