Is there a robot in your patients’ future? Or even more mind-boggling-will some of your patients wear a robot in the future? “Wearable robots,” or “exoskeletons,” are moving out of the realm of science fiction and into the real world, with a variety of applications.
 |
| Exohiker™. Photograph courtesy of Berkeley Bionics. |
Fueled by creative imaginations coupled with technological expertise, wearable robotic applications are springing up all over the world. Military applications can turn ordinary people into “super soldiers” with the ability to carry far more weight faster, farther, and for longer periods of time than is possible for humans alone. Exoskeletons can protect wearers from enemy fire and chemical attack. Some can even enable their wearers to fly! By increasing speed, strength, and protection, these “wearable robots” can help rescue workers more effectively dig people out from under rubble after earthquakes or carry them from burning buildings while protecting the rescuers from falling debris and collapsing structures. Exoskeletons can help nurses to move patients and protect industrial and construction workers from back injuries while lifting heavy loads.
Robotic technology offers promise in the rehabilitation field as well, enabling persons with various disabilities to achieve greater function and mobility. This article will open a window to just a few of these technologies being developed around the world.
Berkeley Bionics
A recent force driving exoskeleton development has been a U.S. Defense Advanced Projects Agency (DARPA) program known as Exoskeletons for Human Performance Augmentation (EHPA).
A prominent result is the Berkeley Lower Extremities Exoskeleton (BLEEX), developed by the University of California, Berkeley. Berkeley Bionics™ was founded to develop commercial applications of the exoskeleton technology. One example is its ExoHiker™, which weighs 31 pounds, including power unit, batteries, and onboard computer. It operates with virtually imperceptible noise, according to Berkeley Bionics website (www.berkeleybionics.com). With lithium polymer batteries, the device can travel 42 miles per pound of battery at a speed of 2.5 miles per hour. With a small, pack-mounted solar panel, “its mission time will be unlimited,” according to the company.
The ExoHiker enables wearers to carry 150 pounds without feeling the load on their shoulders and features retractable legs, quick-release emergency egress from the backpack and/or exoskeleton, and unfettered driving while using the device. Berkeley Bionics latest exoskeleton-HULC™ (Human Universal Load Carrier)-can carry even more, 200 pounds, and decreases the wearer’s oxygen consumption by 15 percent.
A medical adaptation of the Berkeley technology and other similar technologies may enable wheelchair users to walk, possibly even for hours at a time, depending on their condition. It could give users a measure of mobility and help them avoid the onset of wheelchair-related secondary conditions. Wheelchair users, especially those whose wheelchair use has spanned decades, are at risk for diabetes, obesity, and cardiovascular conditions due to a sedentary lifestyle, plus pain resulting from overuse of upper-limb muscles.
Homayoon Kazerooni, PhD, a professor at the University of California, Berkeley, and founder of and the Advanced Technology Program (ATP) project manager for Berkeley Bionics, is enthusiastic about developing the technology for medical use. “It’s not just about walking,” Kazerooni stresses. “It’s also about being able to sit and turn without help; it’s about being able to don and doff the exoskeleton without help. If the person still has to depend on others for assistance in these activities, he or she is not really independent in their mobility.”
Kazerooni says he expects the technology to be commercially available within 18-24 months. He notes, however, that the exoskeleton technology is not for everyone. “I don’t want to give false hope to people with very limited mobility.” Kazerooni also stresses that adequate funding is needed if this technology is to experience rapid advances.
Japan’s HAL 5
 |
| Robot Suit HAL™. Photograph courtesy of Professor Sankai, CYBERDYNE Inc./University of Tsukuba. |
A research team led by Yoshiyuke Sankai, PhD, a professor in the Department of Intelligent Interaction Technologies at Tsukuba University, Tsukuba, Japan, has developed the Robot Suit® Hybrid Assistive Limb (HAL)™ exoskeleton for applications in rehabilitation and physical training support, activities of daily living (ADL) assistance for disabled persons, heavy-labor support for workers, and rescue support for emergency disaster personnel.
CYBERDYNE®, a company created to commercialize the technology, says that HAL can magnify a person’s strength by two times or more. The suit detects “faint biosignals on the surface of the skin when the human brain tries to move the exoskeleton,” Sankai said in an interview on the CYBERDYNE website. When the Robot Suit detects the signals, it helps the user to move, and this information is then relayed back to the brain. “This interactive spiral loop of the human and the robot/ information system is what I think will be the core to develop the next generation [of assistive technologies],” Sankai said.
Sankai was honored by the Lemelson-MIT Program for the HAL robotic suit. Commenting on the award, the program noted, “The latest version, HAL 5, was preceded by prototypes HAL 3 and HAL 4, and with each iteration the system has become lighter and more efficient. Newer HALs include a smaller, wireless connected computer that fits in a pouch attached to a belt, smaller motor housings and better comfort for the wearer. In its latest form, it weighs approximately 15kg or 33 lb. in the lower-body-only model, and 24kg or 55 lb. in the all-body model. It is battery-powered.”
The program continues, “Sankai has said that one of his aims is to create technologies that are designed for the benefit of humankind rather than for destructive purposes. He refused, for example, an offer from the U.S. Department of Defense in Washington DC to work on a robot for military use and declined a similar offer from the government of South Korea.”
MIT Exoskeleton
 |
| Raytheon Sarcos employees try to keep up with software engineer Rex Jameson as he uses the exoskeleton to load a pallet during a demonstration. Photographs courtesy of Raytheon. |
The Massachusetts Institute of Technology (MIT) Media Lab Biomechatronics Group has developed an exoskeleton that can support up to 80 percent of an 80-pound load and which requires only two watts of electrical power during loaded walking. Headed by Hugh Herr, PhD, associate professor, Media Arts and Sciences, MIT-Harvard Division of Health Sciences and Technology and director of the MIT Biomechatronics Group, the concept behind the design “seeks to exploit the passive dynamics of human walking in order to create lighter and more efficient exoskeleton devices,” according to a paper by Herr and Aaron M. Dollar, PhD, titled “Lower Extremity Exoskeletons and Active Orthoses: Challenges and State-of-the-Art,” published in IEEE Transactions on Robotics,
Vol. 24, No. 1, February 2008. “The quasi-passive design does not use any actuators for adding power at the joints. Instead, the design relies completely on the controlled release of energy stored in springs during the (negative power) phases of the walking gait. The quasi-passive elements in the exoskeleton (springs and variable damper) were chosen based on an analysis of the kinetics and kinematics of human walking.”
“However,” the paper continues, “metabolic studies with the quasi-passive exoskeleton showed a 10-percent increase in walking metabolic cost of transport, or the metabolic energy required to transport unit weight unit distance, for a subject carrying the 36kg load via the quasi-passive exoskeleton versus a standard laden backpack. In a separate study, the U.S. Army Natick Soldier Center showed that load-carriage using another quasi-passive exoskeleton design increased metabolic cost of transport on average across three tested loading conditions (20, 40, and 55kg) by as much as 40 percent. To our knowledge, no one has yet demonstrated an exoskeleton that reduces the metabolic cost of transport when compared to the load-carriage with a standard backpack.”
On a positive note, further experimental work showed a significant reduction in metabolic cost of walking versus using the same MIT exoskeleton without the springs at the hip and ankle and the variable damper at the knee, thus demonstrating the utility of the quasi-passive elements.
Sarcos
 |
| Photograph courtesy of Raytheon. |
One of the most talked-about technologies in the popular press is the Sarcos exoskeleton, developed by Stephen Jacobsen, PhD, whose Salt Lake City, Utah-based company, Sarcos, was acquired by Raytheon in 2007. The exoskeleton enables a user to carry a person on his or her back or lift 200 lb. several hundred times without tiring, according to the Raytheon website (www.raytheon.com). The DARPA-funded technology, recently transitioned to the U.S. Army, could potentially have future civilian applications, including rehabilitation applications.
Challenges
“There are still many kinks that must be worked out before HAL or any other exoskeleton become part of everyday life,” points out an article in
Scientific American,
April 30, 2008. The article, “Real- Life Iron Man: A Robotic Suit That Magnifies Human Strength,” by Larry Greenemeier, describes one challenge as the sheer diversity of medical needs exoskeletons must meet. He quotes Herr: “One [person] might have knee and ankle problems, others might have elbow problems…. How in the world do you build a wearable robot that accommodates a lot of people?”
There are also concerns that the exoskeleton could actually hinder rehabilitation by doing all the work of damaged limbs, Greenemeier points out, again quoting Herr: “If the orthotic does everything, the muscle degrades, so you want the orthotic to do just the right amount of work.”
Robotic In-Lab Gait Therapy
Although not as dazzling as the exoskeletons that enable users to perform superhuman feats, robotic applications used only in a clinic or laboratory setting can-and do-aid persons with various neurological and orthopedic conditions in improving their functioning and mobility. Following is an overview of four of these applications.
University of Michigan Robotic AFO and KAFO
 |
| University of Michigan robotic AFO. Photograph courtesy of the University of Michigan. |
Generally, robotic rehabilitative devices move the patients limb by receiving instructions programmed into a computer. The repetitive movement patterns are thought to help the brain and spinal cord work together to reroute signals interrupted by injury or illness.
The University of Michigan robotic devices take the opposite approach: electrical signals received from electrodes attached to the wearers leg are translated into movement by the exoskeleton. Rather than the device moving the patient, the patient moves the orthosis.
“If you think about it, these types of devices would move your legs in a pattern even if you were asleep or unconscious,” points out Daniel Ferris, PhD, associate professor, School of Kinesiology, associate professor, Department of Biomedical Engineering, director of the University’s Human Neuromechanics Laboratory. “Learning requires conscious, active participation.”
He continues, “If you have trouble actuating your muscles because of weakness or impaired signals, it is hard to know when you send the right commands to your muscles because you are not getting feedback on which movements are good and which are not. So when the robotic brace amplifies the strength of the signals and amplifies the effect of their own activation, it helps them discern when they have a correct muscle activation pattern. By practicing with the brace, they learn the right way to recruit their muscles, so that when the brace is removed, they can maintain that pattern.”
 |
| A patient is strapped to the LOPES exoskeleton. Photograph courtesy of the University of Twente. |
Learning how to recruit the right muscle movement patterns is how we learn and improve skills involving our neuromuscular system, such as learning to play tennis or improving our golf swing. In a paper titled “Powered Lower Limb Orthoses for Gait Rehabilitation,” co-authored by Gregory S. Sawicki, MSME, and Antoinette R. Domingo, MPT, published in Topics in Spinal Cord Injury Rehabilitation , November 2005, Ferris states that rehabilitation after neurological injury relies on three principles of motor learning: practice–more learning will occur with more practice; specificity–the best way to improve performance of a motor task is to execute that specific task; and effort–individuals need to maintain a high degree of participation and involvement to facilitate motor learning.
“These three principles are critical to promoting activity-dependent plasticity (i.e., altering the efficacy and excitation patterns of neural pathways by activating those pathways)…. Plasticity occurs in neural pathways that are active. Thus, maximizing neuromuscular recruitment during task-specific practice increases the potential for plasticity.”
Ferris explains how the system works: the AFO and KAFO record muscle activation signals captured through electrodes placed on the skin and send the signals through a computer for signal processing. The computer then controls the pressure regulator in the artificial pneumatic muscle, and it activates a mechanical assistance. The mechanical output from the orthosis is generated at the same time as the mechanical output from the leg muscles.
The robotic AFO is currently undergoing a clinical trial involving eight subjects with incomplete spinal cord injury. Following the completion of this trial in 2010, Ferris hopes to conduct trials under the auspices of the National Institutes of Health (NIH) in multiple centers around the country. In the future, he foresees the technology benefiting stroke survivors and cerebral palsy patients as well.
“We are not interested in making the device portable because we don’t want it to become a long-term substitute for what the human does. We want to use it as a tool to increase the capacity of the human to have better command of his or her own abilities,” Ferris says.
LOPES Project
 |
| Close up of the LOPES bouden cable-driven series elastic actuator. Photograph courtesy of the University of Twente. |
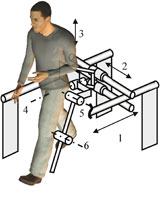
The LOPES (LOwer-extremity Powered ExoSkeleton) is designed to help stroke survivors regain walking ability. Developed in the Laboratory of Biomechanical Engineering at the University of Twente, Enschede, the Netherlands, the LOPES provides eight actuated degrees of freedom (DOF) by means of series elastic actuation.
The device combines a freely translatable and two-dimensional actuated pelvis segment with a leg exoskeleton containing three actuated rotational joints: two at the hip and one at the knee, according to a paper titled “Design and Evaluation of the LOPES Exoskeleton Robot for Interactive Gait Rehabilitation, by J.F. Veneman et al., published in the
IEEE Transactions on Neural Systems and Rehabilitation Engineering
, September 2007.
“The joints are impedance-controlled to allow bidirectional mechanical interaction between the robot and the training subject. Evaluation measurements show that the device allows both a ‘patient-in-charge’ and ‘robot-in-charge’ mode, in which the robot is controlled either to allow or to guide a patient, respectively.”
EMG measurements on eight important leg muscles show that free walking in the device strongly resembles free treadmill walking-“an indication that the device can offer task-specific gait training.”
 |
| Schematic of the LOPES bouden cable-driven series elastic actuator. Photograph courtesy of the University of Twente. |
Growing scientific evidence shows that task-specific, intensive training of actively performed movements results in the largest function improvement, notes the University of Twente website (www.bw.ctw.utwente.nl/research/projects/lopes.doc/index.html). However, providing this training is very labor-intensive for physical therapists. An aging population that is producing more patients, coupled with an expected decrease in the number of therapists, exacerbates the situation. “By using robotic devices to provide the patient with the required support, these problems can be circumvented,” the website notes.
Clinical trials are currently under way, according to Herman van der Kooij, PhD, associate professor of Biomechatronics at the University of Twente and LOPES project coordinator. According to Kooij, the technology is expected to be commercially available within two years.
Lokomat
Developed in 2000 by Hocoma, a Swiss-based medical technology company, the Lokomat® is available in several U.S. locations, including the Rehabilitation Institute of Chicago (RIC), Illinois. RIC began clinical trials of robot-assisted walking therapy with the Lokomat in 2002, when it was first approved by the U.S. Food and Drug Administration (FDA).
 |
| Schematic overview of the degrees of freedom that the LOPES provides. Photograph courtesy of the University of Twente. |
The Lokomat can assist persons whose ability to walk has been impaired by brain or incomplete spinal cord injury, stroke, multiple sclerosis, hip replacement, or other neurological and orthopedic conditions. The device works by suspending the patient in a harness over a treadmill while the robots frame, which is attached by straps to the outside of the legs, moves the legs in a natural walking pattern. A computer controls the pace of walking and measures the bodys response to the movement. In addition to training the brain and spinal cord, benefits of walking therapy can include strengthening muscles, improving circulation, and strengthening bones at risk for osteoporosis.
Like the LOPES, the Lokomat can lighten the load for physical therapists. Without robotic assistance, walking therapy is usually performed with the aid of two or more physical therapists who manually move the patients legs in a walking pattern; however, the labor intensity, strenuous nature, and variability of this method can limit the frequency and duration of therapy, points out the RIC website (www.ric.org). “With robot-assisted walking therapy, the robotic device does most of the heavy work, the pattern and pace are consistent throughout the session, and the exercise can be sustained over longer periods of time.”
A Robot in Your Practices Future?
This is only a glimpse of robotic technologies being researched and developed-with some now or soon to be commercially available. In the future, will one of these technologies provide a brighter, better, more functional lifestyle for some of
your
patients?
Miki Fairley is a contributing editor for
The O&P EDGE
and a freelance writer based in southwest Colorado. She can be contacted via e-mail at
[email protected]
Companies, other organizations, and products are included in this article for informational purposes only.
The O&P EDGE
does not endorse any products or services.
Rochester Institute of TechnologyRobotic assistive and rehabilitative technologies are not limited to lower-limb applications. Research is being conducted and robotic technologies are being developed for upper-limb rehabilitation as well. For instance, researchers at the Biomechatronic Learning Laboratory at the Rochester Institute of Technology (RIT), New York, are conducting research on human-robot interfaces for an upper-limb robotic orthosis to help muscular dystrophy patients increase function. |




