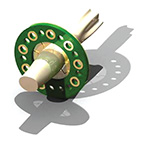
The device, which looks like a wagon wheel with open spaces between the “spokes,” allows the nerve to grow.
Photograph courtesy of Dan Moran, PhD.
Daniel Moran, PhD, a Washington University in St. Louis (WashU) professor of biomedical engineering in the School of Engineering & Applied Science and of neurobiology, physical therapy, and neurological surgery in the School of Medicine, has received a three-year, nearly $1.9 million grant from the Defense Advanced Research Projects Agency (DARPA) to test a novel device developed in his lab that would stimulate the nerves in the upper arm and forearm. If it works, people with upper-limb amputations who use motorized prosthetic devices would be able to feel various sensations through the prosthesis, which would send sensory signals to the brain.
DARPA has already funded a high-tech bionic limb created by DEKA Research and Development, Manchester, New Hampshire. The prosthesis, dubbed the “Luke Skywalker” or “Luke” arm, is designed to help service members and veterans who have upper-limb amputations. While the advanced prosthetic arm allows users to perform six different grips, such as for picking up small objects, it does not provide users with the senses of touch and orientation of a natural hand-which is what DARPA’s Hand Proprioception and Touch Interfaces (HAPTIX) program aims to address.
Moran, whose expertise is in motor neurophysiology and brain-computer interfaces, and his team have developed an electrode-a macro-sieve peripheral nerve interface-that is designed to stimulate sensory nerve cells in the ulnar and median nerves in the arms. The ulnar nerve, one of three main nerves in the forearm, is the largest nerve in the body unprotected by muscle or bone and is connected to the ring finger and pinkie finger on the hand, and is the nerve that is stimulated when the “funny bone” is triggered. The median nerve in the upper arm and shoulder is connected to the other fingers on the hand, so together the two nerves control movement and sensations including touch, pressure, vibration, heat, cold, and pain in all of the fingers.
The device, which is made of an ultrathin, flexible material similar to a soft contact lens and is about one-eighth the size of a dime, will be implanted into the forearms of anesthetized primates. The research team will then determine the amount of sensory information that is encoded by providing low levels of stimulation to small groups of nerves. A small cuff electrode will also be implanted to compare the performance.
Once implanted, Moran said he and the team will train the primates to play a joystick-controlled video game in which the researchers will give cues as to where the primates should move the joystick by stimulating specific sectors in the ulnar and median nerves so it feels as if someone is touching them. “We want to determine what they can perceive through artificial stimulation of the nerves,” Moran said. “Using very low levels of stimulation (i.e. sensation), we want to figure out how many different nerve sectors we can independently encode with a unique target location…[and] how small we can make the stimulation so they can still sense it.”
In particular, Moran and the team will analyze how many different independent channels they can stimulate on the nerve to determine how many sensors will work on the prosthetic hand. They will then work with DARPA to determine how many sensors to put on the prosthetic hand.
“If the nervous system can’t handle more than eight or ten channels, there is no sense in putting more on there,” Moran said. “We want to find the bandwidth and what the nervous system can interpret with artificial sensation.”
Editor’s note: This story was adapted from materials provided by Washington University in St. Louis.




